Sciatica is an umbrella term for anything that involves the sciatic nerve. It could be inflammation around the nerve itself, it might be a compression from a disc, or a narrowing where the nerve passes through, it is often tightness in muscles also that restrict the movement in the nerve, there are many causes to sciatica but it is usually describing pain down the back or outside of the leg / buttock which may or may not come with back pain.
Symptoms:
-
You might have pain / tingling / numbness in the:
-
Back (on one or both sides).
-
Hip / buttock.
-
Outside of or back of the thigh.
-
Outside or back of the lower leg.
-
Ankle / foot.
-
-
You might have weakness in the affected leg.
-
Your back pain is often less pronounced than the leg symptoms.
-
The leg / buttock pain is often described as a ‘toothache’ type pain.
-
The symptoms might worsen when you move from one position to another or cough / sneeze.
-
Difficulty walking / standing or sitting for long periods.
Causes:
-
Herniated disc (likely present prenatally).
-
‘Wear and tear’ to the spine bones causing some compression on the nerves (this would have been present before pregnancy and is less likely to be the cause of the increase in symptoms. If symptoms don’t settle after the birth then this is something that could be looked into but an MRI scan would be needed.
-
Increased muscle tension in pregnancy.
-
Unstable or looser joints due to hormone changes in pregnancy.
-
Weight gain from the growing baby and the babies position.
-
Weakness (abdominal region in particular) as the belly muscles stretch with the growing baby, causes excess stress on the lower back and nerves.
-
Rectus Abdominis separation (diastasis recti), also associated with weakness and extra pressure on the lower back and the nerves associated with that region (see also Diastasis Recti section).
-
History of back pain (pre-pregnancy or in other pregnancies).
-
Changes in posture, adding pressure to the spine in the lower back.
-
Stress can also cause increased muscle tone, changes in posture and extra pressure on the spine and nerves in the lower back.
-
Change in exercise habits.
Here is what the latest evidence says about treatment for sciatica:
Exercise – This study found that exercise helped to reduce the risk of low back pain and therefore rates of sick leave in pregnant women and this study compared exercise with no exercise and found that prenatal exercise decreased the severity of low back pain and pelvic girdle pain during and following pregnancy.

Yoga – evidence suggests that yoga is a safe and very effective method in the treatment of back pain and sciatica. This systematic review found strong evidence for short-term effectiveness and moderate evidence for long-term effectiveness of yoga for chronic low back pain.
There are lots of Online Yoga programmes available, have a look at our Top 5 here (and why we love them)! You can also read our blog on how yoga can help in other ways.

Pilates – This study strongly supports the use of Pilates in various back pain issues. Have a look at our top 5 online Pilates options here.
Swimming – There has been quite a lot of research into the effectiveness of swimming, when it comes to nerve pain or injury (particularly sciatica), unfortunately a lot of the studies are animal based (but results have been promising). This study showed positive results when swimming was used to help repair nerves and this human based, systematic review, reported that aquatic exercise can significantly reduce pain and increase physical function in patients with low back pain.
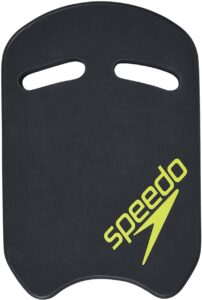
If you want to try swimming but don’t consider yourself a strong swimmer, try a kickboard. A kickboard is a float that you hold which allows you to use your legs only (and you can swim easily without putting your head in the water). Using a kickboard also allows you to do a front-crawl leg kick or use a ‘narrower’ breaststroke leg kick (which can help if you have pelvic girdle pain). You can buy a kickboard at a really reasonable price here.
TENS – evidence is in support of the use of TENS machines for lower back issues in pregnancy. Always speak to your midwife or GP before using a TENS machine to check it is the right course of action for you (and your baby).
There are many different TENS machines available to buy, so if you are thinking of TENS as a treatment option then have a look at our Top 5 picks to make things a little easier.
Pregnancy Support Belt – evidence is available for the use of support belts in pregnancy. THIS study concluded that wearing a support belt during pregnancy can have beneficial effects such as; reduced lower back pain and pelvic girdle pain, improvement of functionality and mobility and reduction of risk of fall during pregnancy.
There are no studies to show which support belts work best or for how long you should be wearing them, so we have put together our top 5 choices (here) to help guide you based on what they can help with and what we like about them.
Pregnancy support Pillow – There is little evidence in support of the pregnancy pillow. That’s not to say that it doesn’t work, it just means that there hasn’t been a need to carry out studies on them. A pregnancy pillow aims to help keep your spine and hips in a neutral position whilst lying on your side. I know from personal experience that they are very comfortable and can double up as a feeding pillow once the baby is born, I think they’re a good investment but whether they will help to alleviate back pain and or sciatica – the jury is still out on that one.
Have a look at out Top 5 pregnancy pillows available here.
Kinesio Tape –evidence is good for the use of K-Tape in lower back pain during pregnancy, we couldn’t find specific studies that backed its use in sciatica but the general ‘offloading’ principles should help any associated symptoms.
HERE is a video on how you would apply the tape to the back and THIS is the tape we usually recommend (based on reviews).
Trigger point release – This is a technique used to relieve tension in muscles, it can provide some really instant relief to symptoms of sciatica and pain in the buttocks. Have a look at THIS post by our friends over at Finola Physio for tips on how to carry this out yourself. You just need a fairly solid ball like a tennis ball or a spiky ball like this one which is reasonably priced (and is usually a good investment for any future issues you might have).
Acupuncture – THIS study found that, compared with bed rest, acupuncture might be an effective and acceptable strategy to relieve symptoms of postpartum sciatica. Please contact your local Physiotherapist and ask if they are qualified in acupuncture treatments (AACP approved) to try this form of treatment.

Doughnut cushions – a lot of studies have been carried out in order to check the effects of doughnut cushions on pressure relief. The studies are always in their favour, so if pain is an issue in sitting then something like this might help to take some of the pressure off the affected area. Various types of cushions are on the market, have a look at our Top 5 pressure relief cushions HERE.

Symptoms to watch out for:
If you have any of the following symptoms then speak to your GP right away or go to your nearest accident and emergency department immediately:
-
Severe low back pain.
-
Pain, numbness, or weakness in one or both legs that causes you to stumble or have trouble getting up from a chair.
-
Loss of or altered sensations in your legs, buttocks, inner thighs, feet or areas that you sit on when in a chair (including genitals / anus) that is severe or gets worse and worse.
-
Recent problem with bladder or bowel function, such as trouble eliminating urine or waste (retention) or trouble holding it (incontinence).
-
Sexual dysfunction that has come on suddenly.
Cauda Equina Syndrome is a very rare but very serious condition that must be addressed immediately to prevent any lasting damage to the nerves involved. You may have one of the above symptoms of a number of these symptoms. Report any changes to your GP / Midwife immediately.
-
Severe pain at night (usually in the legs) causing disturbed sleep.
-
Pain and numbness in the leg at rest and/or while walking.
-
Pain relief experienced mainly while sitting on a chair with the feet hanging down.
-
Pronounced swelling in the feet and ankles (often pregnancy related so speak to your health care provider if this happens).
-
Pale colour and less warmth in the skin over the toes and feet compared to the legs.
Acute Limb Ischemia is a condition which occurs due to decreased or loss of blood supply to the legs. Leg pain in acute limb ischemia may feel similar to sciatica pain. It is essential that you seek help for the above symptoms as soon as possible to aid your recovery and prevent any long term damage.